Cervical cancer expained!
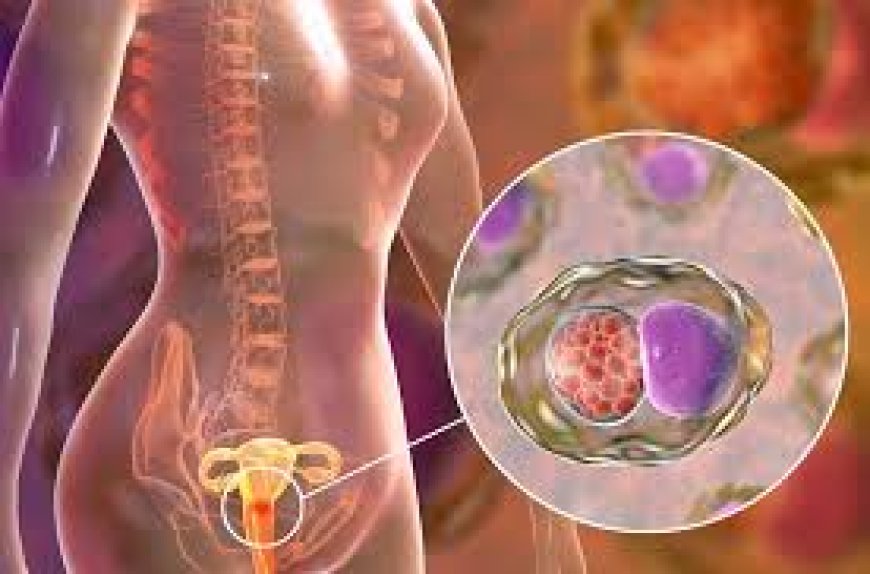
Cervical cancer originates from the cells of the cervix, the lower portion of the uterus connecting it to the vagina. Typically, it progresses gradually, beginning with dysplasia, wherein abnormal cervical cells emerge. If left untreated, these aberrant cells may evolve into cancer cells, spreading deeper into the cervix and adjacent areas. The two primary types of cervical cancer are squamous cell carcinoma, arising from ectocervical cells, and adenocarcinoma, which develops in endocervical glandular cells. Occasionally, a hybrid form, known as adenosquamous carcinoma, combines features of both types. Human papillomavirus (HPV) infection, particularly persistent strains, is the primary cause of cervical cancer. Symptoms include post-coital bleeding, postmenopausal bleeding, abnormal vaginal bleeding, unusual vaginal discharge, and pelvic discomfort or pain during intercourse.
Various factors contribute to the risk of cervical cancer:
1. Smoking: Tobacco use heightens the risk of cervical cancer by prolonging HPV infections, which are the primary cause of most cervical cancers.
2. Sexual Activity: The more sexual partners one has, and the more partners each of those individuals has had, the higher the likelihood of HPV transmission, thus increasing the risk of cervical cancer.
3. Sexually Transmitted Infections (STIs): Contracting other STIs elevates the risk of HPV infection, thereby raising the likelihood of developing cervical cancer. STIs such as herpes, chlamydia, gonorrhea, syphilis, and HIV/AIDS are implicated in this heightened risk.
4. Weakened Immune System: Individuals with compromised immune systems due to underlying health conditions are at a greater risk of developing cervical cancer if infected with HPV.
5. Prenatal Exposure to Medication: In cases where a parent was administered diethylstilbestrol (DES), a medication aimed at preventing miscarriages during pregnancy, there is a potential increased risk of cervical cancer, particularly clear cell adenocarcinoma, due to its historical use in the 1950s.
To mitigate the likelihood of cervical cancer:
1. Consult Your Healthcare Provider Regarding the HPV Vaccine: Inquire with your doctor about the HPV vaccine as a preventive measure against HPV infections, thereby potentially decreasing the risk of cervical cancer and other HPV-related cancers. Seek guidance from your healthcare team to determine if the HPV vaccine is appropriate for you.
2. Undergo Regular Pap Tests: Regular Pap tests are essential for detecting precancerous cervical conditions, allowing for timely monitoring or intervention to prevent the onset of cervical cancer. Most medical bodies recommend initiating routine Pap tests at age 21 and undergoing periodic screenings thereafter.
3. Adopt Safe Sexual Practices: Minimize your risk of cervical cancer by practising safe sex methods to prevent sexually transmitted infections. This involves consistent condom use during sexual activity and limiting the number of sexual partners you engage with.
Each year, over 12,000 women are diagnosed with cervical cancer, a largely preventable disease, with up to 93% of cases avoidable. Vaccination against human papillomavirus (HPV) prevents infections linked to most cervical cancers. Approximately 13,820 new cases of invasive cervical cancer are expected annually, resulting in about 4,360 fatalities. While cervical pre-cancers are frequently detected, invasive cervical cancer diagnoses are less common. Typically, cervical cancer affects women aged 35 to 44, with the average age of diagnosis being 50, seldom occurring in those under 20. Despite this, many older women are unaware of their continued susceptibility to cervical cancer, with over 20% of cases occurring in women over 65, albeit rare in those who undergo regular screening. Although cervical cancer incidence rates declined significantly from the mid-1970s to the mid-2000s due to increased screening, they have since stabilized. However, rates have risen by 1.7% annually from 2012 to 2019 in women aged 30-44 while declining by 11% annually for those aged 20-24, possibly reflecting the impact of HPV vaccination on cancer prevention. Once a leading cause of cancer death among American women, the cervical cancer death rate has halved since the mid-1970s, primarily due to prevention and screening efforts. However, rates have plateaued in recent years. Notably, the death rate is approximately 65% higher in Black and Native American women compared to White women.
Ways to raise awareness about cervical cancer include leveraging Cervical Cancer Awareness Month in January, where the focus is on ending cervical cancer within a few generations. Early detection and effective management significantly increase treatment success rates, even for late-stage diagnoses. A holistic approach encompassing prevention, screening, and treatment can effectively combat cervical cancer as a public health issue within a few generations. Critical actions for awareness include getting informed about cervical cancer and HPV, encouraging screening starting at age 30, advocating for HPV vaccination for girls aged 9 to 14, and setting up information booths at various venues such as hospitals, schools, and community events. Additionally, advocacy efforts can involve education through social media, public speaking engagements, and organizing informational events. Community leaders can participate in health fairs, conferences, and awareness activities. Workplace initiatives can also play a role by educating employees on cancer risk factors, promoting healthy lifestyles, and supporting cessation efforts for smoking. The World Health Organization (WHO) has set a goal to eliminate cervical cancer as a public health issue globally by 2120, with interim targets to be achieved by 2030, including high HPV vaccination rates, increased screening, and improved treatment accessibility. Regional strategies, tailored to diverse cultural, social, and economic contexts, aim to complement global efforts toward cervical cancer elimination.
Treatment options for cervical cancer vary, and your healthcare team will collaborate with you to devise a personalized plan, often combining different approaches based on factors such as cancer stage, overall health, and personal preferences. Your treatment plan will outline details about your cancer, treatment goals, available options, potential side effects, and duration. If fertility preservation concerns arise, discussing them with your healthcare team before treatment initiation is advisable. Oncologists, specialized cancer care doctors, and multidisciplinary teams comprising various healthcare professionals like nurses, social workers, and therapists collaborate to formulate comprehensive treatment strategies. Patient involvement in shared decision-making is crucial, where discussions with doctors about treatment goals and expectations help tailor care to individual needs. Understanding the potential impacts on sexual function and fertility is vital and should be addressed before treatment commences, especially for pregnant individuals whose treatment may be postponed until after childbirth. Common treatment modalities for cervical cancer include surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy, with supportive care for managing symptoms and side effects integral to the overall care plan. Further information on treatment options by cancer stage, managing metastatic disease, achieving remission, and addressing potential recurrence are also essential considerations.











































